Introduction
Angioplasty is a medical procedure used to treat blockages in the arteries that supply blood to the heart. It is a minimally invasive technique that can significantly improve blood flow to the heart muscle, reducing the risk of heart attacks and other cardiovascular complications. In this comprehensive article, we will explore the various aspects of angioplasty, including its types, benefits, procedures, risks, recovery process, and prevention strategies.
Types of Angioplasty
There are several types of angioplasty procedures, each tailored to address specific cardiovascular issues:
● Coronary Angioplasty: This is the most common form of angioplasty, used to treat coronary artery disease (CAD) by opening narrowed or blocked coronary arteries. CAD occurs when fatty deposits, known as plaques, build up in the coronary arteries, reducing blood flow to the heart.
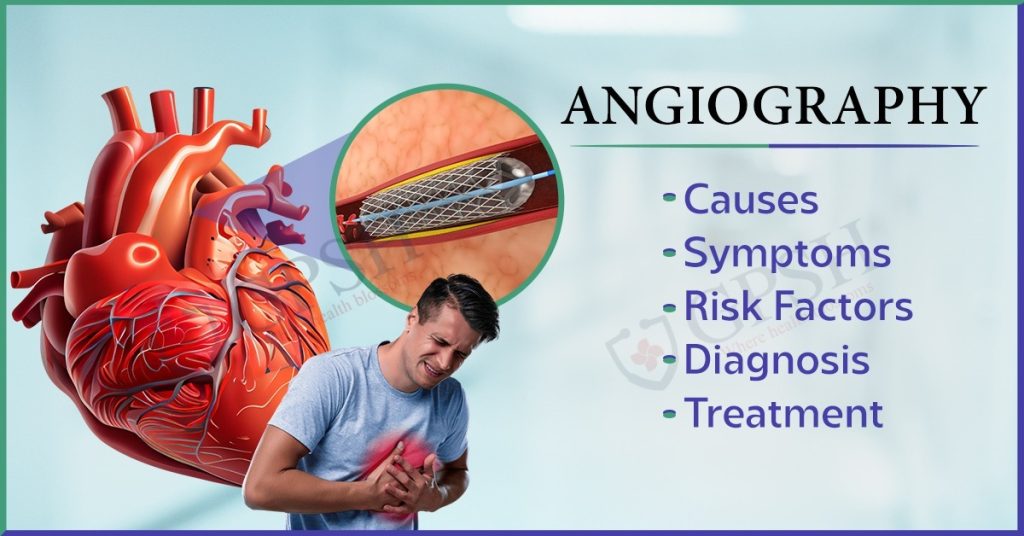
● Balloon Angioplasty: During this procedure, a small balloon is inflated inside the blocked artery to widen it and restore normal blood flow. The inflation of the balloon compresses the plaque against the artery walls, creating a larger opening.
● Stent Placement: Stents are often used alongside balloon angioplasty. These tiny mesh tubes are inserted into the artery to keep it open, reducing the risk of re-narrowing. Stents can be coated with medication to further prevent restenosis.
● Peripheral Angioplasty: Peripheral arteries in the legs, arms, or other parts of the body can also become blocked due to atherosclerosis. Peripheral angioplasty is used to improve blood flow in these areas, alleviating symptoms such as leg pain and cramping.
You Can Read also:- Multiple Myeloma: Symptoms, Causes, Diagnosis and Treatment
Benefits of Angioplasty
Angioplasty offers numerous benefits for individuals with blocked arteries:
● Improved Blood Flow: Angioplasty effectively opens blocked arteries, restoring blood flow to the heart and reducing the risk of heart attacks. Improved blood flow can also relieve angina (chest pain) and other related symptoms.
● Symptom Relief: Patients often experience relief from symptoms such as chest pain (angina) and shortness of breath after angioplasty. This improved quality of life is a significant benefit.
● Lowered Risk of Complications: By improving blood flow, angioplasty can reduce the risk of serious heart-related complications, including heart attacks and heart failure.
● Minimally Invasive: Angioplasty is less invasive than traditional open-heart surgery, resulting in shorter hospital stays and quicker recovery times. Most patients can return to their normal activities within a short period.
Procedure of Angioplasty
The angioplasty procedure is typically performed in a cardiac catheterization laboratory (cath lab) and follows these steps:
● Preparation: The patient is prepped, and a local anesthetic is administered to numb the area where the catheter will be inserted, which is usually in the groin or wrist.
● Catheter Insertion: A thin, flexible catheter with a deflated balloon at its tip is threaded through an artery to reach the blocked area. The choice of access point depends on the location and severity of the blockage.
● Angiography: A contrast dye is injected through the catheter, and X-ray images are taken to visualize the blockage and its location within the coronary arteries. This imaging helps the interventional cardiologist plan the procedure.
● Balloon Inflation: The balloon at the catheter’s tip is inflated to compress the plaque against the artery walls, widening the passage for blood flow. The pressure applied by the balloon is carefully controlled to avoid damaging the artery.
● Stent Placement: If necessary, a stent may be implanted during the procedure to support the artery and maintain its openness. Some stents are drug-eluting, releasing medication over time to prevent restenosis (re-narrowing of the artery).
● Deflation and Catheter Removal: After the successful treatment, the balloon is deflated, and the catheter is carefully withdrawn. The stent remains in place to provide ongoing support.
● Recovery: The patient is closely monitored for a short time in the recovery area to ensure there are no immediate complications. Most patients can return to a regular hospital room shortly after the procedure.
You Can Read also:- Ehrlichiosis: Causes, Symptoms, Risk Factors, Diagnosis and Treatment
Risks of Angioplasty
While angioplasty is generally safe and effective, it does carry certain risks and potential complications, including:
● Bleeding and Bruising: Minor bleeding and bruising at the catheter insertion site are common but usually resolve quickly. However, excessive bleeding may require additional medical intervention.
● Infection: There is a slight risk of infection at the insertion site. Proper sterilization procedures are followed to minimize this risk.
● Blood Clots: Blood clots can form at the stent site, potentially causing complications. To prevent this, patients are often prescribed blood-thinning medications.
● Artery Damage: In rare cases, the catheter may cause damage to the artery, leading to bleeding or blood vessel injury. Highly skilled interventional cardiologists take precautions to minimize this risk.
● Allergic Reactions: Some patients may have an allergic reaction to the contrast dye used during the procedure. Medical personnel are trained to manage such reactions promptly.
● Kidney Problems: The contrast dye used in angiography can affect kidney function, especially in individuals with pre-existing kidney issues. Patients with kidney problems may require special precautions or alternative imaging techniques.
● Restenosis: Although stents are effective at keeping arteries open, there is a risk of restenosis, where the artery narrows again over time. Drug-eluting stents, coated with medication, are often used to reduce this risk.
Recovery of Angioplasty
Recovery from angioplasty varies from person to person but generally involves:
● Hospital Stay: Most patients can go home the same day or the day after the procedure. However, some individuals with complex conditions may need a longer hospital stay.
● Medications: Patients are often prescribed a regimen of medications, including antiplatelet drugs (such as aspirin and clopidogrel) and blood thinners, to prevent blood clots and reduce the risk of restenosis. Compliance with medication is crucial for long-term success.
● Lifestyle Changes: Adopting a heart-healthy lifestyle is essential for a successful recovery. This includes dietary improvements, regular exercise, smoking cessation, and alcohol moderation. These changes can reduce the risk of future blockages and cardiovascular events.
● Follow-up Care: Regular follow-up appointments with a cardiologist are essential to monitor progress and adjust medications if necessary. These visits also allow the healthcare team to address any concerns or complications that may arise.
● Return to Normal Activities: Patients can usually resume normal activities within a week or two, although strenuous exercise may need more time. The recovery period may vary depending on the individual’s overall health and the complexity of the procedure.
Prevention of Angioplasty
Preventing the need for angioplasty is a primary goal of heart health. To reduce the risk of arterial blockages and cardiovascular issues, consider the following prevention strategies:
● Maintain a Healthy Lifestyle: Eat a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Regular exercise, such as brisk walking or swimming, helps maintain a healthy weight and promotes cardiovascular health. Avoid smoking and excessive alcohol consumption, as they contribute to heart disease.
● Manage Chronic Conditions: Control high blood pressure, diabetes, and high cholesterol through medication and lifestyle changes. Regularly monitor your blood pressure, blood sugar, and cholesterol levels as recommended by your healthcare provider.
● Regular Check-ups: Schedule regular check-ups with a healthcare provider to monitor your heart health and catch potential issues early. Routine screenings can help detect risk factors and conditions that may lead to arterial blockages.
● Medication Adherence: If you are prescribed medications for heart-related conditions, take them as directed by your healthcare provider. Skipping doses or discontinuing medications without medical guidance can increase the risk of heart problems.
● Stress Management: Practice stress-reduction techniques such as meditation, yoga, or deep breathing exercises. Chronic stress can contribute to heart disease, so finding healthy ways to manage stress is crucial.
Conclusion
In conclusion, angioplasty is a life-saving procedure that effectively treats blocked arteries, reducing the risk of heart attacks and improving overall heart health. While it carries some risks, the benefits of angioplasty are substantial, including symptom relief and improved blood flow. Recovery involves lifestyle changes, medication management, and follow-up care to maintain long-term heart health. To avoid the need for angioplasty, it’s crucial to prioritize heart-healthy habits and manage chronic conditions through regular medical supervision. By taking proactive steps, individuals can significantly reduce the likelihood of developing arterial blockages and related cardiovascular issues.