White Spots on Tonsils: Causes, Symptoms, Treatment, and Risks
You might be concerned about a serious illness if you notice white spots on your tonsils. White spots, however, have several causes, and they aren’t always treatable with medicine.
Antibiotics may occasionally be required to treat an infection that results in white patches on the tonsils. Your tonsils may need to be medically removed by a tonsillectomy in specific circumstances.
This page discusses the typical causes of white spots on the tonsils, additional symptoms to look out for, how these spots are typically treated, and when you should consult a doctor about them.
What are White Spots on the Tonsils?
White spots on the tonsils may appear to be a straightforward and minor issue, but it is advised against ignoring them as the infection could worsen and spread. You should consult a doctor to avoid further difficulties as occasionally this can lead to a major injury.
Some of the on points, conspicuous signs that would warn you of white spots on the tonsil include swollen glands on the neck, a dry and sore throat, white spots at the back of the throat, an unpleasant taste in the mouth, and, enlarged tonsils.
Causes of White Spots on Tonsils
The emergence of white patches in the neck is typically a sign of a bacterial or viral infection. Common infections that might cause white throat patches to include the following.
1. Strep throat
One of the most typical causes of sore throat, particularly in kids, is strep throat. White pus streaks on the tonsils are one sign of strep throat.
The group A Streptococcus bacteria cause strep throat. It can spread when near or in direct contact with someone who has a strep infection because it is highly contagious.
Some symptoms of strep throat include:
● Tonsil swelling and redness
● There is sometimes a white patch or a streak of pus on the tonsils
● Suffering from swallowing pain
● Throat soreness suddenly
● The temperature is above 100.4°F (38°C)
● Swelling of the lymph nodes around the neck’s front
2. Tonsillitis
Tonsils that are inflamed or swollen are referred to as tonsillitis. A bacterial infection, such as strep throat, may cause this. Tonsillitis is more frequently brought on by a viral infection. Tonsillitis is quite frequent among children, much like strep throat.
Some symptoms of tonsillitis include:
● Inflammation of the throat, ranging from mild to severe
● Symptoms of red and swollen tonsils
● Tonsils with white or yellow patches
● An unpleasant odor of smell
● Pain in swallowing food
● The temperature is above 100.4°F (38°C)
● Swelling of the lymph nodes around the neck’s front
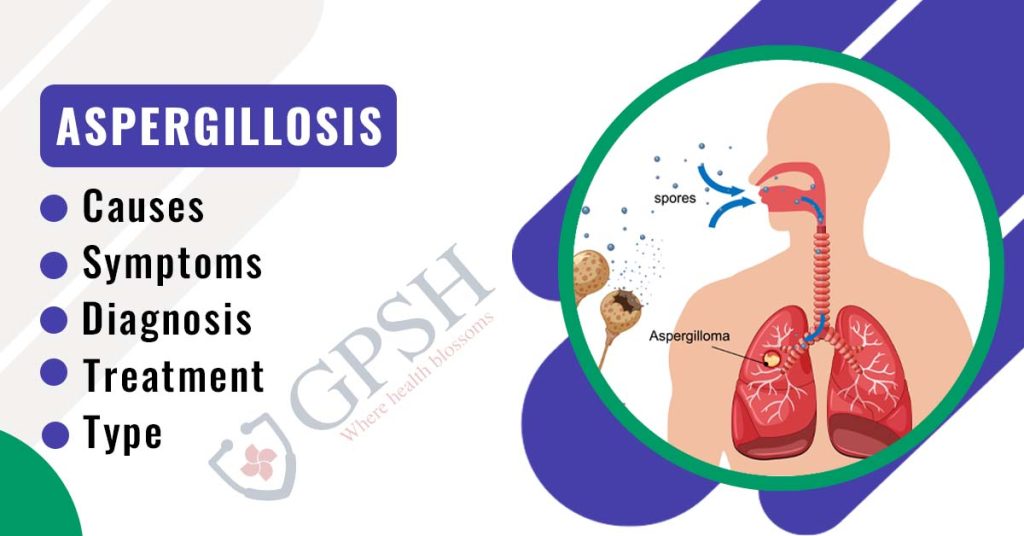
You Can Also Read:- Aspergillosis: Types, Causes, Symptoms, Diagnosis & Treatment
3. Oral thrush
Oral candidiasis, an infection of the mouth and throat brought on by Candida albicans, is also known as oral thrush. Including in the mouth and throat, the fungus Candida albicans develops naturally in the body.
Oral candidiasis, on the other hand, can arise when this fungus overgrows, frequently as a result of a compromised immune system. This might be the result of an acute problem or a transient one, like taking antibiotics.
Some symptoms of oral thrush include:
● The throat and oral cavity both have white spots in them.
● Cottony sensation in the mouth
● Throat discomfort
● Swelling and erythema
● Swallowing difficulty
● Taste loss
4. Mononucleosis
Epstein-Barr virus (EBV) infections, also known as mono or mononucleosis, are the most common cause of this illness. Ages 15 to 24 are the group where it occurs most frequently. After being exposed to EBV, symptoms may not appear for 4-6 weeks.
Some symptoms of mononucleosis include:
● Extreme fatigue
● Sore throat
● Swollen tonsils that could have white patches on them
● Lymph nodes in the neck and under the arms that are swollen
● A temperature of at least 100.4 °F (38 °C)
Symptoms of White Spots on Tonsils
Numerous other symptoms, which differ depending on the cause of the spots on your tonsils, are frequently accompanied by white spots on your tonsils. These may include:
● Sore throat
● Neck lymph nodes (glands) that are enlarged
● The voice is strained
● Fever
● Difficulty swallowing
● Red and enlarged tonsils
● Your mouth’s roof is covered in tiny red spots.
● Possible extreme exhaustion
● Body aches and headaches
● Rashes
● Taste loss
● Having difficulty swallowing or eating
● Your mouth’s corners are cracked and discolored.
● Bad breath
● Ear pain
● The most typical symptom of tonsillitis with white spots is a sore throat.
Risk Factors of White Spots on Tonsils
White spots on the tonsils are more likely to appear in people with compromised immune systems.
Various conditions have different risk factors. For instance, living close to others can make it more likely for you to contract mono and strep throat.
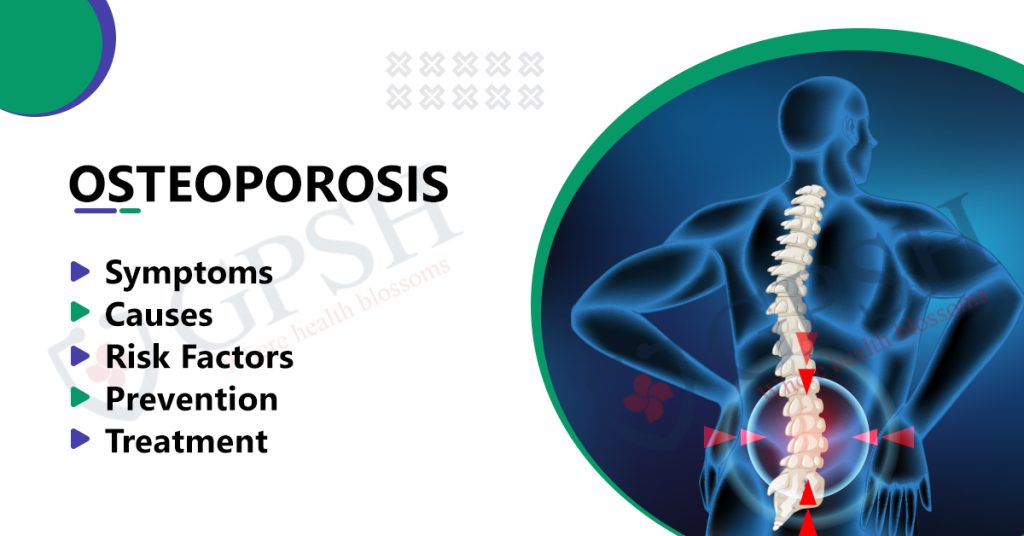
You Can Also Read:- Osteoarthritis: Symptoms, Causes, Prevention, Diagnosis, and Treatment
When should I see a doctor?
If your child exhibits symptoms that could point to tonsillitis, it’s critical to get a proper diagnosis.
If your child exhibits any of the following, contact your doctor right away:
● fever and a sore throat
● a persistent sore throat that lasts longer than 24 to 48 hours
● difficulty swallowing or discomfort
● excessive sluggishness, exhaustion, or fussiness
Diagnosis of White Spots on Tonsils
A doctor will:
● Examine the throat’s back.
● Check the neck area for any swelling.
● Examine other symptoms that you have.
Additionally, they could swab the throat or draw blood for laboratory analysis. These can indicate the presence of bacteria, and if they do, doctors may then advise taking antibiotics.
Treatment of White Spots on Tonsils
Depending on what caused the white spots, you may need different treatments.
For infectious mononucleosis
To treat mono, doctors rarely recommend medications. For severe inflammation, your doctor may also recommend over-the-counter drugs like ibuprofen in addition to corticosteroids.
Careful home care will be your best course of treatment. While the infection is healing, drink plenty of water and get plenty of rest. If you have an enlarged spleen, stay away from contact sports.
For strep throat
An antibiotic will be recommended by your doctor. For pain relief and swelling reduction, your doctor may also advise over-the-counter drugs like ibuprofen (Advil, Motrin IB).
Take your medication and get plenty of rest as well. You might also give gargling with warm salt water a try; it can help to lessen pain and swelling.
For oral thrush
For the treatment of thrush, doctors typically recommend antifungal drugs. It might be possible to stop the yeast from spreading outside of your mouth by gargling with salt water and washing your mouth with water.
For tonsil stones
Unless the discomfort is severe, treatment for tonsil stones is typically not required. The stones will be naturally removed by your body. To remove the deposits, you can try DIY techniques like eating crackers or other crunchy foods and spritzing salt water. its.
For severe inflammation
Your doctor might advise having your tonsils removed if they are so inflamed that doing so makes it difficult for you to breathe.
A tonsillectomy is a medical term for this procedure. Usually, it’s only applied after trying other methods without success to lessen tonsil inflammation. It wouldn’t only be used to treat white spots, according to your doctor.
The best time to have a tonsillectomy is after a disease has been treated. There is a higher risk of bleeding if they are done while you are infected, but this only happens very rarely.
Usually performed as an outpatient procedure, tonsillectomies. For one to two weeks following the procedure, you’ll probably have a sore throat.
Other treatments for White Spots on the Tonsils
Home remedies can be used to treat any kind of sore throat, but they should only be used in conjunction with medical care. These merely hasten to heal and alleviate symptoms. You can attempt some of the following:
● Gargling with warm water mixed with salt or lemon, water, and honey;
● Teas made with honey that include ginger, eucalyptus, mauve, salvia, or althea;
● Consuming grapefruit juice. If you are currently taking medication that was prescribed to you by your doctor, you should avoid drinking grapefruit juice because it might make the medication less effective.
● Resting and consuming plenty of fluids are crucial during treatment because they will speed up the body’s recovery.
White Spots on Tonsils: Causes, Symptoms, Treatment, and Risks Read More »