Post-Delivery Weight Loss: Your Journey to a Healthier You
Introduction
After giving birth, many women are concerned about their weight and the process of losing the weight gained during pregnancy.
Weight Gain During Pregnancy: During pregnancy, it is normal and healthy for women to gain weight. The amount of weight gained varies depending on factors such as pre-pregnancy weight, overall health, and individual circumstances. On average, women may gain between 25 to 35 pounds (11 to 16 kilograms) during pregnancy, but this can vary.
Weight Loss Immediately After Delivery: After giving birth, women typically experience immediate weight loss. This weight loss is primarily due to the expulsion of the baby, placenta, and amniotic fluid.
Additionally, the body sheds some of the retained fluids, which can contribute to weight reduction. On average, women may lose around 10 to 12 pounds (4.5 to 5.5 kilograms) immediately after delivery. It’s important to understand that post-delivery weight loss is a gradual process and may take time.
Be Patient with Yourself
Absolutely! It’s crucial to be patient and kind to yourself when it comes to post-delivery weight loss. Here are some reasons why you need to be patient:
1. Physical Recovery: Your body has gone through significant changes during pregnancy and childbirth. It needs time to heal and recover. Rushing into intense weight loss efforts immediately after delivery may not be healthy or sustainable. Giving yourself time to physically recover will allow your body to regain strength and energy.
2. Hormonal Changes: Hormonal fluctuations after childbirth can affect your body’s metabolism and weight regulation. It’s important to let your hormones stabilize naturally, which can take several weeks or even months. Being patient during this time will help your body find its balance.
3. Prioritizing Your Baby: After delivery, your focus shifts to taking care of your newborn. It’s crucial to prioritize your baby’s needs, including feeding, sleep, and overall care. This can leave less time and energy for rigorous weight loss activities. Being patient with yourself allows you to establish a healthy routine and gradually incorporate self-care activities.
4. Sustainable and Healthy Weight Loss: Rapid weight loss is not always healthy or sustainable. It’s better to focus on gradual and steady weight loss, which is more likely to lead to long-term success. By allowing yourself time, you can adopt healthier habits, such as a balanced diet and regular exercise, that promote sustainable weight loss.
5. Emotional Well-being: The postpartum period can bring about a range of emotions, and it’s important to prioritize your emotional well-being. Putting unnecessary pressure on yourself to lose weight quickly can add stress and negatively impact your mental health. Being patient allows you to focus on self-care and bonding with your baby, which is essential for your overall well-being.
Remember, every woman’s journey is unique, and there is no specific timeline for post-delivery weight loss. It’s important to be kind to yourself, celebrate small victories, and seek support from your healthcare provider, family, and friends. Embrace the process and focus on your overall health and well-being as you gradually work towards your weight loss goals.
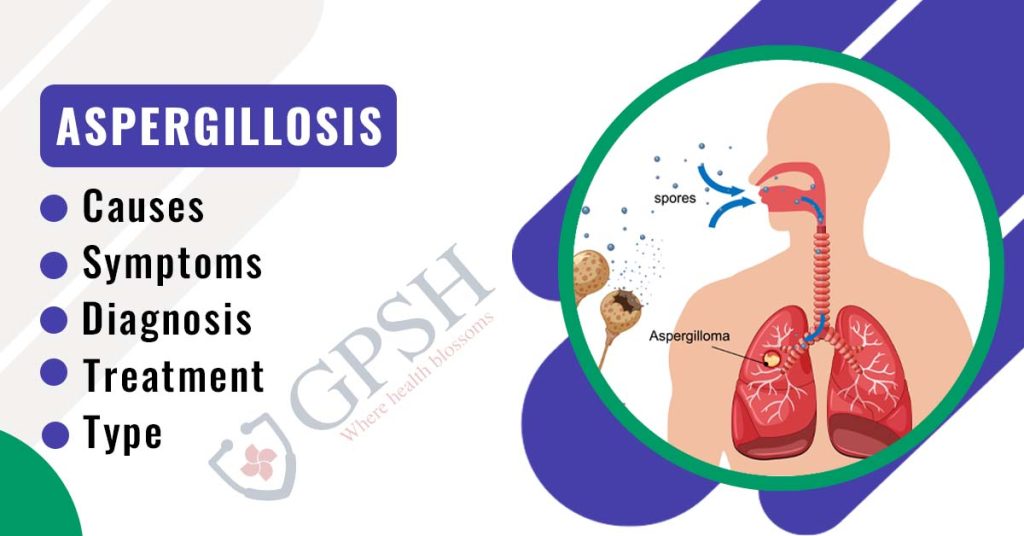
You Can Also Read:- Aspergillosis: Types, Causes, Symptoms, Diagnosis & Treatment
Nourish Your Body
Post-delivery body nourishment is crucial for the overall health and well-being of a new mother.:
1. Balanced Nutrition: Focus on consuming a well-balanced diet that includes a variety of nutrient-dense foods. Include sources of lean proteins, whole grains, fruits, vegetables, healthy fats, and dairy or dairy alternatives. This will provide the necessary nutrients to support your recovery and breastfeeding if applicable. Consult with a healthcare provider or a registered dietitian for personalized nutrition advice.
2. Adequate Hydration: Staying hydrated is essential, especially if you are breastfeeding. Aim to drink plenty of fluids throughout the day, such as water, herbal teas, and fresh fruit juices. Adequate hydration helps maintain your energy levels, supports milk production, and aids in overall body function.
3. Nutrient Foods: Choose foods that are rich in nutrients. Include sources of iron, calcium, folate, omega-3 fatty acids, and vitamins such as A, C, and D. Incorporate foods like leafy greens, legumes, lean meats, fish, eggs, nuts, seeds, and whole grains to ensure you are getting a wide range of nutrients.
4. Postpartum Supplements: Your healthcare provider may recommend specific supplements to support your postpartum recovery. These may include a prenatal or postnatal multivitamin, omega-3 fatty acids, or vitamin D supplements. Follow your provider’s guidance on appropriate supplements based on your individual needs.
5. Gradual Weight Loss: If you’re looking to lose weight after delivery, it’s important to focus on gradual and sustainable weight loss. Rather than resorting to restrictive diets, prioritize nourishing your body with wholesome foods. Gradually incorporate physical activity, as approved by your healthcare provider, to support weight loss and overall well-being.
6. Listen to Your Body: Pay attention to the signals of hunger and fullness that your body sends you. Eat when you’re hungry and stop when you’re satisfied. Postpartum can be demanding, and it’s important to fuel your body adequately. Additionally, be mindful of any food sensitivities or allergies and avoid foods that may cause discomfort.
7. Rest and Self-Care: Adequate rest is essential for postpartum recovery. Aim to get enough sleep and rest whenever possible. Self-care activities, such as taking relaxing baths, practicing deep breathing exercises, and engaging in activities that bring you joy, can also contribute to your overall well-being.
You Can Also Read:- When to Take Creatine? Best Time to take Creatine
Breastfeeding Role in Post-Delivery body changes and weight loss
Breastfeeding plays a significant role in post-delivery body changes and weight loss for many women. Here’s how breastfeeding can impact your body and aid in weight loss:
1. Calorie Expenditure: Breastfeeding requires energy, as the body uses calories to produce breast milk. On average, breastfeeding can burn around 300-500 extra calories per day. This calorie expenditure can contribute to weight loss over time, as the body taps into stored fat reserves to meet the increased energy demands.
2. Uterine Contractions: Breastfeeding stimulates the release of the hormone oxytocin, which causes the uterus to contract. These contractions can help the uterus return to its pre-pregnancy size more quickly. As the uterus shrinks, it can lead to a reduction in the belly area, contributing to overall postpartum weight loss.
3. Fat Stores Utilization: When you breastfeed, your body prioritizes the production of breast milk, which relies on the use of stored fat reserves. This means that some of the fat accumulated during pregnancy may be utilized to produce milk, aiding in weight loss.
4. Hormonal Impact: Breastfeeding affects hormone levels, including prolactin. Prolactin promotes milk production and has been associated with the suppression of ovulation. Delayed ovulation can lead to a delay in the return of the menstrual cycle, which can impact weight loss for some women.
5. Appetite Regulation: Breastfeeding can help regulate your appetite. Some women find that they experience a natural increase in hunger while breastfeeding, while others may notice a decrease in appetite. This can vary individually. Listening to your body’s hunger and fullness cues is important to ensure adequate nourishment without overeating.
Remember, maintaining a well-balanced diet, staying adequately hydrated, and engaging in regular physical activity (as approved by your healthcare provider) alongside breastfeeding can further support postpartum weight loss. Be patient with yourself, focus on overall health, and consult with your healthcare provider or a lactation consultant for personalized guidance on breastfeeding and weight loss.
Physical activities to incorporate after Post-Delivery
Incorporating physical activity after post-delivery can be beneficial for your overall health, well-being, and postpartum recovery. However, it’s important to consult with your healthcare provider before starting any exercise routine to ensure it is safe and appropriate for your specific situation. Here are some physical activities that are often recommended for post-delivery:
1. Walking: Including walking in your daily routine is a simple way to engage in low-impact exercise. Start with short, leisurely walks and gradually increase the duration and intensity as you feel comfortable. Walking can help improve cardiovascular fitness, boost mood, and aid in weight loss.
2. Pelvic Floor Exercises: Strengthening the pelvic floor muscles is important after childbirth. Pelvic floor exercises, commonly known as Kegel exercises, help to restore muscle tone and support the pelvic organs. Consult with a healthcare provider or a physical therapist for guidance on proper technique and progression.
3. Postnatal Yoga or Pilates: Postnatal yoga or Pilates classes specifically designed for new mothers can be beneficial for strengthening and toning the body, improving flexibility, and promoting relaxation. These exercises often focus on core strength, posture, and breathing techniques. Look for classes or videos that are suitable for postpartum women.
4. Low-Impact Aerobics: Low-impact aerobics classes or workouts can provide cardiovascular benefits without placing excessive stress on the joints. Look for classes or exercises that are specifically designed for postpartum women or consider low-impact activities such as swimming or stationary cycling.
5. Strength Training: Incorporating strength training exercises with light weights or resistance bands can help rebuild muscle strength and tone your body. Focus on exercises that target major muscle groups, including squats, lunges, modified push-ups, and bicep curls. Start with lighter weights and gradually increase as your strength improves.
6. Mom and Baby Classes: Look for fitness classes specifically designed for new moms that allow you to bring your baby along. These classes often involve exercises that incorporate your baby, such as baby-wearing workouts or exercises done while holding your baby. It’s a great way to bond with your baby while getting some exercise.
Conclusion
In conclusion, post-delivery weight loss is a gradual process that varies for each woman. It’s important to approach weight loss after childbirth with patience, kindness, and a focus on overall health. Here are key points to remember:
1. Gradual and Sustainable: Aim for gradual and sustainable weight loss rather than rapid results. Healthy weight loss typically ranges from 1-2 pounds (0.5-1 kg) per week.
2. Balanced Nutrition: Focus on a well-balanced diet that includes nutrient-dense foods. Consume lean proteins, whole grains, fruits, vegetables, and healthy fats, and stay adequately hydrated.
3. Breastfeeding Benefits: Breastfeeding can aid in weight loss as it burns extra calories and stimulates uterine contractions. However, the extent of weight loss varies, and the primary focus should be on providing nourishment for your baby.
4. Physical Activity: Incorporate physical activity gradually after receiving approval from your healthcare provider. Activities like walking, postnatal yoga, low-impact aerobics, and strength training can support postpartum recovery and weight loss.
5. Rest and Self-Care: Adequate rest, self-care activities, and managing stress are essential for postpartum well-being. Prioritize self-care and listen to your body’s needs.
6. Individual Variations: Each woman’s postpartum weight loss journey is unique. Factors such as genetics, metabolism, breastfeeding, and overall health play a role. Focus on your progress and avoid comparing yourself to others.
Remember, post-delivery weight loss is not the sole measure of success. Embrace the changes your body has gone through and celebrate the strength and resilience it took to bring new life into the world. Consult your healthcare provider for personalized guidance, and be patient and kind to yourself throughout the process. Your health and well-being, as well as that of your baby, should be the top priority.
Post-Delivery Weight Loss: Your Journey to a Healthier You Read More »