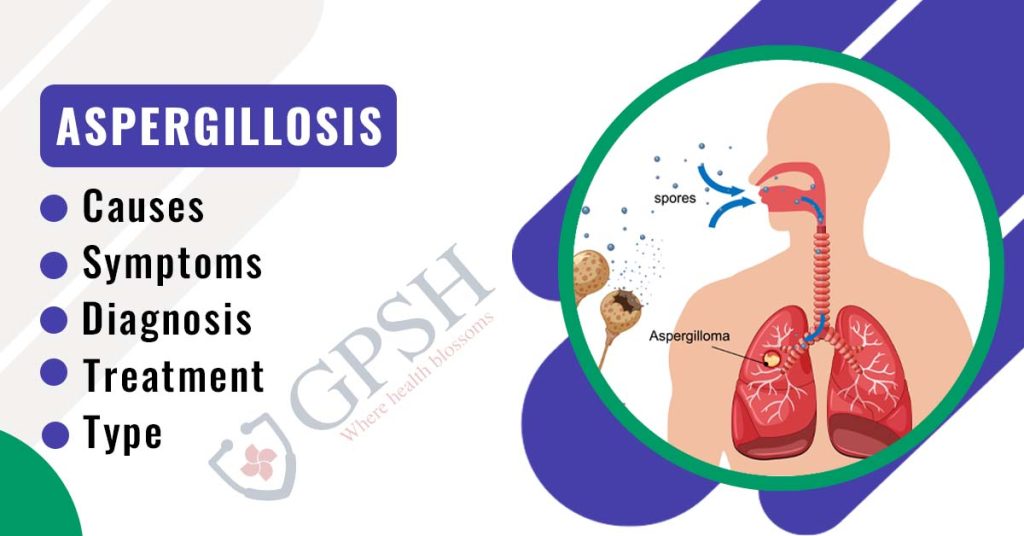
Aspergillosis: Types, Causes, Symptoms, Diagnosis & Treatment
An infection called aspergillosis is brought on by a particular kind of mold (fungus). The respiratory system is typically affected by aspergillosis-related illnesses, but the symptoms and severity of these conditions can differ greatly.
Aspergillus, a type of mold, is present both indoors and outdoors and is the cause of the illnesses. The majority of these mold strains are not harmful, but a few of them can be harmful to those with compromised immune systems, underlying lung conditions, or asthma when they inhale their fungus spores.
Some people develop an allergic reaction when exposed to spores. Some individuals experience minor to severe lung infections. When the infection spreads to blood vessels and beyond, it becomes invasive aspergillosis, the most dangerous type of the condition.
Observation, antifungal drugs, or, in rare circumstances, surgery may all be used as treatments for different types of aspergillosis.
What is Aspergillosis?
Aspergillosis is an infection caused by the Aspergillus fungus, an allergic reaction, or a fungal growth.
The decaying vegetation and dead leaves are a food source for the fungus. Aspergillosis can develop without any prior exposure to the fungus. The fungus is present in almost everyone’s daily life, but nobody ever gets sick from it.
People with weakened immune systems are more likely to contract infections. It is possible to find Aspergillus indoors and outdoors, the mold responsible for causing infections.
The majority of types of this mold are innocuous when inhaled by persons with compromised immune systems, underlying lung diseases, or asthma, but a few types may cause catastrophic infection.
You can also read:- Osteoarthritis: Symptoms, Causes, Prevention, Diagnosis, and Treatment
Types of Aspergillosis
There are mainly three types of aspergillosis:
1. Pulmonary Aspergillosis
People with damaged lungs or persistent lung conditions are most susceptible to developing this condition. The lungs of these individuals contain unusual spaces where the mold spores that have been inhaled can quickly grow. The fungus can, in a few uncommon instances, also infect the sinuses and ear canals.
2. Invasive Aspergillosis
This form of aspergillosis is the most serious and, if left untreated, can be fatal. It happens when the infection leaves the lungs and enters the bloodstream. Additionally susceptible to infection are various organs like the liver, kidneys, skin, and brain. A weakened immune system, prolonged use of specific corticosteroids, or a low level of white blood cells are some risk factors for invasive aspergillosis.
3. Allergic Bronchopulmonary Aspergillosis (ABPA)
This is an allergic reaction brought on by contact with the Aspergillus fungus. People who have been affected experience inflammation in their lungs and airways. Because they typically have more mucus in their airways, people with asthma, cystic fibrosis, or bronchiectasis are more likely to experience it.
Causes of Aspergillosis
A fungus known as aspergillus is the source of aspergillosis. The fungus is frequently observed growing on decomposing vegetation, such as compost piles, dead leaves, and grain that has been stored. It is also present in marijuana leaves.
Even though aspergillus is something to which most people are frequently exposed, aspergillus infections in immune-suppressed individuals are extremely uncommon.
Aspergillosis can take several different forms:
● An allergy to the fungus can cause allergic pulmonary aspergillosis. People with lung conditions like asthma or cystic fibrosis are more likely to develop this infection.
● A growth (fungus ball) known as an aspergilloma appears where there has previously been scarring or lung diseases, such as from a lung abscess or tuberculosis.
● An infection that causes pneumonia is invasive pulmonary aspergillosis. There is a possibility that other body regions will also be affected. The most common victims of this infection are those with compromised immune systems. This can result from illnesses or medications that reduce the quantity or functionality of white blood cells or impair the immune system, such as cancer, AIDS, leukemia, organ transplants, chemotherapy, and others.
You Can Also Read:- Osteoporosis: Symptoms, Causes, Risk Factors, Prevention and Treatment
Symptoms of Aspergillosis
Although the symptoms of various aspergillosis types vary, the following are some typical ones to look out for:
● Chest and bone pain
● Pneumonia
● Having trouble seeing
● Urethral blood
● Reduced urine
● Headaches
● Chills
● Having trouble breathing
● Coughing while secreting sputum
● Blood in sputum
● Skin sores
● Anorexia and weight loss
How is aspergillosis diagnosed?
The following tests may be prescribed by a doctor to identify aspergillosis:
● Allergy tests. To identify allergic or chronic forms of aspergillosis, your doctor might order skin or blood tests.
● Biopsy. Your healthcare provider might collect tissue or fluid samples to check for indicators of an Aspergillus infection.
● Blood tests. An early diagnosis of invasive aspergillosis in those with severely compromised immune systems can be made with the aid of a blood test.
● Culture. Your healthcare professional may take samples of your bodily fluids, such as blood, mucus (sputum), or the fluid surrounding your lungs, brain, or spinal cord, and attempt to grow Aspergil.
● Imaging. The area of your body that your doctor suspects may be infected may be subjected to X-rays or CT scans to look for Aspergillus symptoms.
How is aspergillosis treated?
Different diseases require different aspergillosis treatments. Possible treatments include:
● Observation. Medications frequently are ineffective at treating simple, isolated aspergillomas, which frequently don’t require treatment. Aspergillomas without symptoms may instead just need to be closely watched by a chest X-ray. The illness may worsen if antifungal drugs are not prescribed.
● Oral corticosteroids. Preventing the worsening of existing cystic fibrosis or asthma is the aim of treating allergic bronchopulmonary aspergillosis. Oral corticosteroids are the most effective way to achieve this. Antifungal drugs by themselves are ineffective for treating allergic bronchopulmonary aspergillosis, but they can be used in conjunction with corticosteroids to lessen the dosage of the latter and enhance lung function.
● Antifungal medications. This drug is suggested as a course of treatment for invasive pulmonary aspergillosis. It is best to take voriconazole (Vfend), a recently developed antifungal medication. Another choice is amphotericin B. All antifungal medications have the potential to cause major side effects, like liver and kidney damage. Antifungal medicine interactions with other medications are also frequent.
● Surgery. When an aspergilloma causes pulmonary bleeding, surgery to remove the fungal mass is the first line of treatment since antifungal drugs don’t penetrate an aspergilloma very well.
● Embolization. By using this procedure, aspergilloma-related lung bleeding is stopped. Material is injected by a radiologist using a catheter that has been inserted into an artery supplying a lung cavity where an aspergilloma is leaking blood. When the substance is injected, it hardens, obstructing the area’s blood supply and putting an end to the bleeding. Although the bleeding is likely to resume after this treatment has worn off.
Prevention for Aspergillois
Mold caused by Aspergillus is difficult to avoid. Consult your provider about the best measures to take if you have a high risk of contracting an infection. Your provider might:
● For infection prevention, prescribe an antifungal medication.
● Check you for infection symptoms so that you can start treatment right away.
Your risk of exposure to fungi may be decreased by:
● Avoiding places like compost piles or construction sites that are heavily polluted with dust or mold.
● Staying away from chores like lawn mowing and gardening. Put on an N95 face mask if you could be exposed to airborne mold or dust.
Aspergillosis: Types, Causes, Symptoms, Diagnosis & Treatment Read More »